Zinc Chelation: A siren song to draw regenerative drugs to the beta cell?
To precisely send a drug to its intended target in the body requires two things: One, the intended target must possess a unique quality that distinguishes it from everything else surrounding it, and two, the drug must be able to recognize and use this unique property to then specifically seek the target alone and nothing else. A recent study by Stanford Diabetes Research Center (SDRC) member Dr Justin Annes’ group did just that: They designed a drug that specifically targets insulin-producing beta cells.
The beta cells of the pancreas are certainly unique. They are the sole source of insulin for the body and there are not very many of them: they form less than 2% of the pancreas, arranged in tiny cell clusters called islets. That is why the body develops diabetes when they are destroyed or functionally impaired. While insulin injections can help ‘manage’ diabetes, more permanent solutions that repair or regenerate the beta cells and enable the body to manage its own insulin demands are highly desirable. For instance, drugs that help beta cells replicate and make more beta cells have been developed but therein lies a challenge. These drugs could cause other cells to divide as well, an unwanted and potentially dangerous side effect. Dr. Annes sought to answer how a therapeutic drug could be specifically delivered to beta cells.
“……we must learn to aim and to aim in a chemical sense.” — Paul Ehrlich, 1963
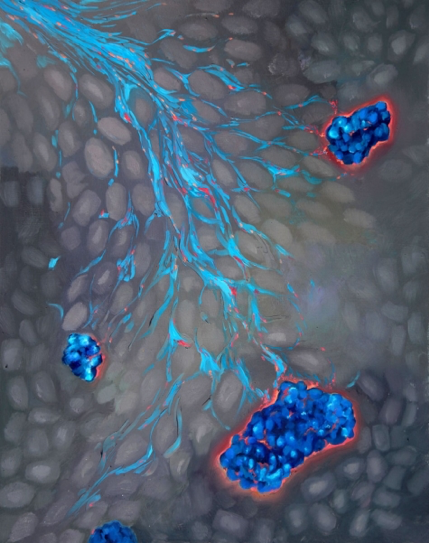
He and his colleagues addressed this challenge by tapping into a unique property of beta cells - a propensity to accumulate zinc within their insulin granules. Beta cells cannot get enough of zinc; indeed, beta cells collect zinc like Imelda Marcos collected shoes! In fact, the amount of zinc in beta cells is a thousand times higher than that of the surrounding cells in the pancreas. Dr Annes hypothesized that if one could design a drug that binds zinc it will thus be irresistibly drawn to the beta cells.
To test this, Dr Annes’ team sought help from two groups - Dr Smith at Stanford ChEM-H to create a new drug compound and the Stanford Islet Research Core of the SDRC to test it in beta cells. First, Dr Horton and Dr Smith worked to create a compound comprised of two components: A Drug (to induce beta cells to divide) and a Zinc Chelator (that anchors to zinc). The next step was to put the drug to the test to determine whether it could be selectively taken up by islet beta cells grown in a dish. Dr Annes’ group found that the beta cells from both rat and human islets did indeed accumulate more of the drug than the surrounding non-beta cells and this effect was dependent on the zinc-accumulating property of the beta cells.
While the finding that drugs can be selectively delivered to beta cells is very exciting, Dr Annes said in a Stanford News Press Release, “This is the first demonstration of a selectively delivered replication molecule in beta cells. It is not sufficient for therapeutic applications”. Indeed, the ability to deliver a drug to the right cells is not in itself a guarantee of drug efficacy. To this point, the researchers found that the effect on the replication of the human beta cells was quite modest even though rodent beta cells responded well. However, the team believes that the approach itself can be adapted to deliver improved treatments to beta cells one day and help cure diabetes.
The SDRC directly supported this study via pilot funding and expertise from the SDRC islet core facility. The lead author of this study published in the December 3, 2018 issue of Cell and Chemical Biology is graduate student Timothy M.Horton. The other co-authors include Dr Paul A. Allegretti, Dr Sooyeon Lee, graduate student Hannah Moeller and Senior Research Scientist, ChEM-H, Dr Mark Smith.
By
Harini Chakravarthy
Harini Chakravarthy is a science writer for the Stanford Diabetes Research Center.