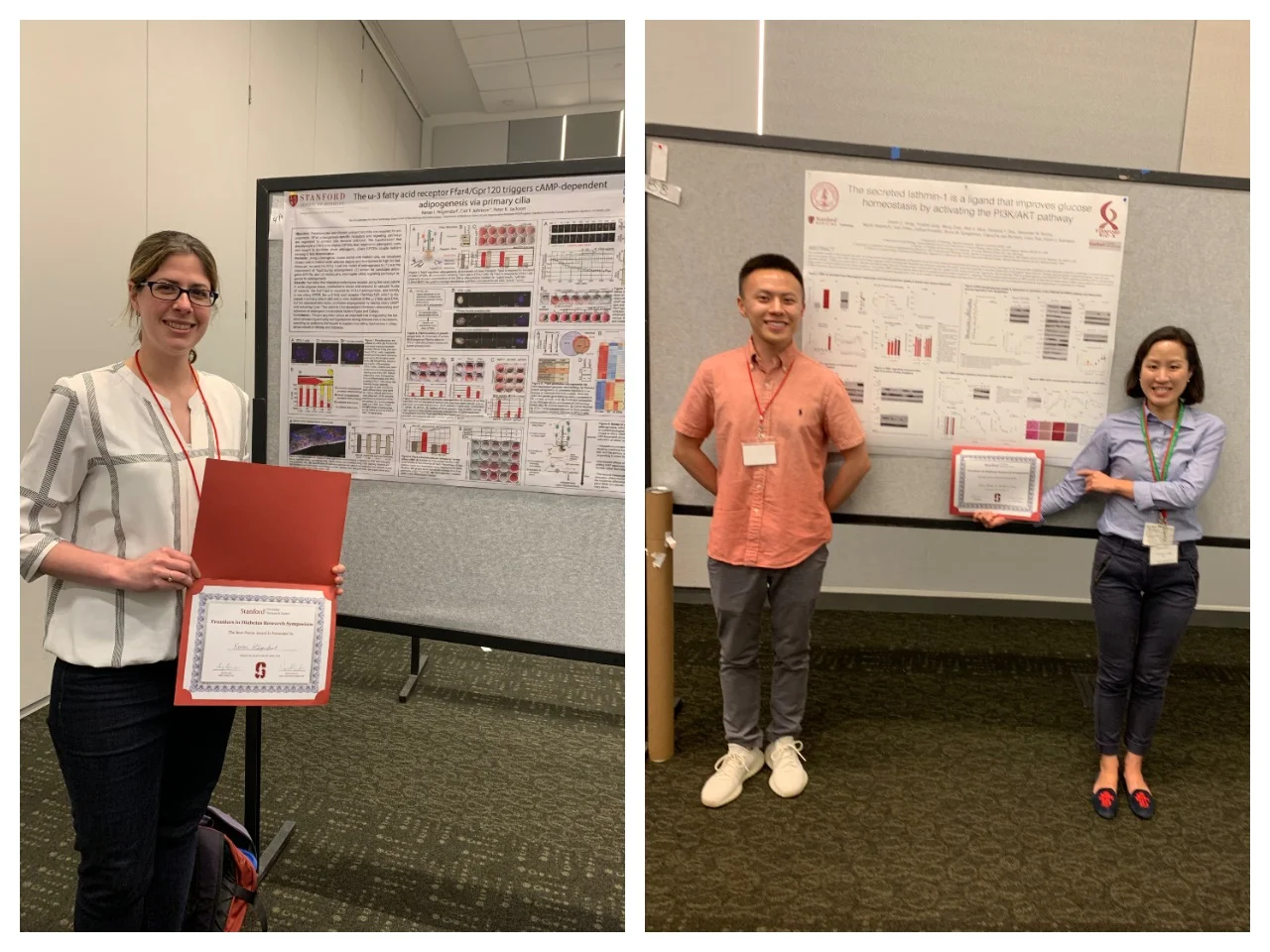
Trainees honored at the 4th Annual Frontiers in Diabetes Research Symposium on April 24th, 2019 with Best Poster Awards!
Keren Hilgendorf (Research Scientist, Jackson lab, Microbiology and Immunology) – “The w-3 Fatty Acid Receptor Ffar4/Gpr120 Triggers Camp-Dependent Adipogenesis via Primary Cilia”
Adipocyte hypertrophy and de novo adipogenesis mediate WAT expansion. Hypertrophy in excess is linked to insulin resistance. Adipogenesis in vitro is induced by insulin, glucocorticoids, and IBMX. However, the physiological signals that activate adipogenesis are poorly defined. Quiescent preadipocytes are uniformly ciliated in vitro, and cilia are important for adipogenesis. Patients with dysfunctional cilia are diabetic and obese. However, the function of ciliary signaling in preadipocytes is unknown. Here, we use a mouse model to show that the primary cilium is an in vivo marker of preadipocytes and critical for initiating adipogenesis. Specifically, 30% of all perivascular cells in fat pads are ciliated, and these ciliated cells are activated in response to HFD. Further, Tulp3, critical for trafficking GPCRs to the primary cilium, is required for adipogenesis. We discovered that Ffar4/Gpr120 is localized to preadipocyte cilia in vitro and in vivo. Addition of Ffar4 ligand, the ω3 fatty acid DHA, activates ciliary Ffar4 and promotes adipogenesis of both 3T3-L1 and primary preadipocytes. Ffar4 activation acutely raises cAMP in the cilium. This in turn activates EPAC, promotes chromatin remodeling, and induces expression of Pparγ. Thus, DHA is a physiologically relevant ligand that replaces the pharmacological agent IBMX to promote adipogenesis, and this requires the primary cilium. These data provide a molecular rationale for the anti-diabetic effects of DHA and explain how ciliary dysfunction causes obesity and diabetes.
Owen Jiang & Yunshin Jung (Research Scientist & Post-doctoral fellow, Svensson lab, Pathology) – “Isthmin-1 Is an Endocrine Activator of the pi3k Pathway That Improves Glucose Homeostasis”
The metabolic benefit of thermogenic fat cells, including brown and beige adipocytes, is thought to arise from both their classical heat generating functions and also their ability to secrete adipokines. Previous work has indicated that thermogenic adipose tissue can crosstalk to liver and other organs, but the specific molecules involved in this crosstalk have not been fully explored. Here, we have identified Isthmin-1 ISM1 as a secreted protein that is highly inducible during adipocyte differentiation. In humans, higher gene expression levels of ISM1 in adipose tissue correlates with increased BMI. Administration of ISM1 protein to or overexpression in obese mice improves insulin sensitivity without causing hypoglycemia, and demonstrate liver and subcutaneous adipose tissue as dominant target organs of ISM1. Phospho-kinase screening identifies that ISM1 is activating the classical PI3K signaling pathway in a similar manner to insulin, but unlike insulin, ISM1 has integrated suppressive actions on both expression of gluconeogenic enzymes and lipogenic genes in liver and hepatocytes. Thus, ISM1 shares the common PI3K/AKT pathway with insulin but can uncouple lipogenesis from gluconeogenesis. Our data identify a new hormone signaling pathway that prevents the development of diabetes and hepatic steatosis with therapeutic potential for the treatment of metabolic diseases.